
Understanding Sleep Tips for Pregnant Women: Key Insights
Share

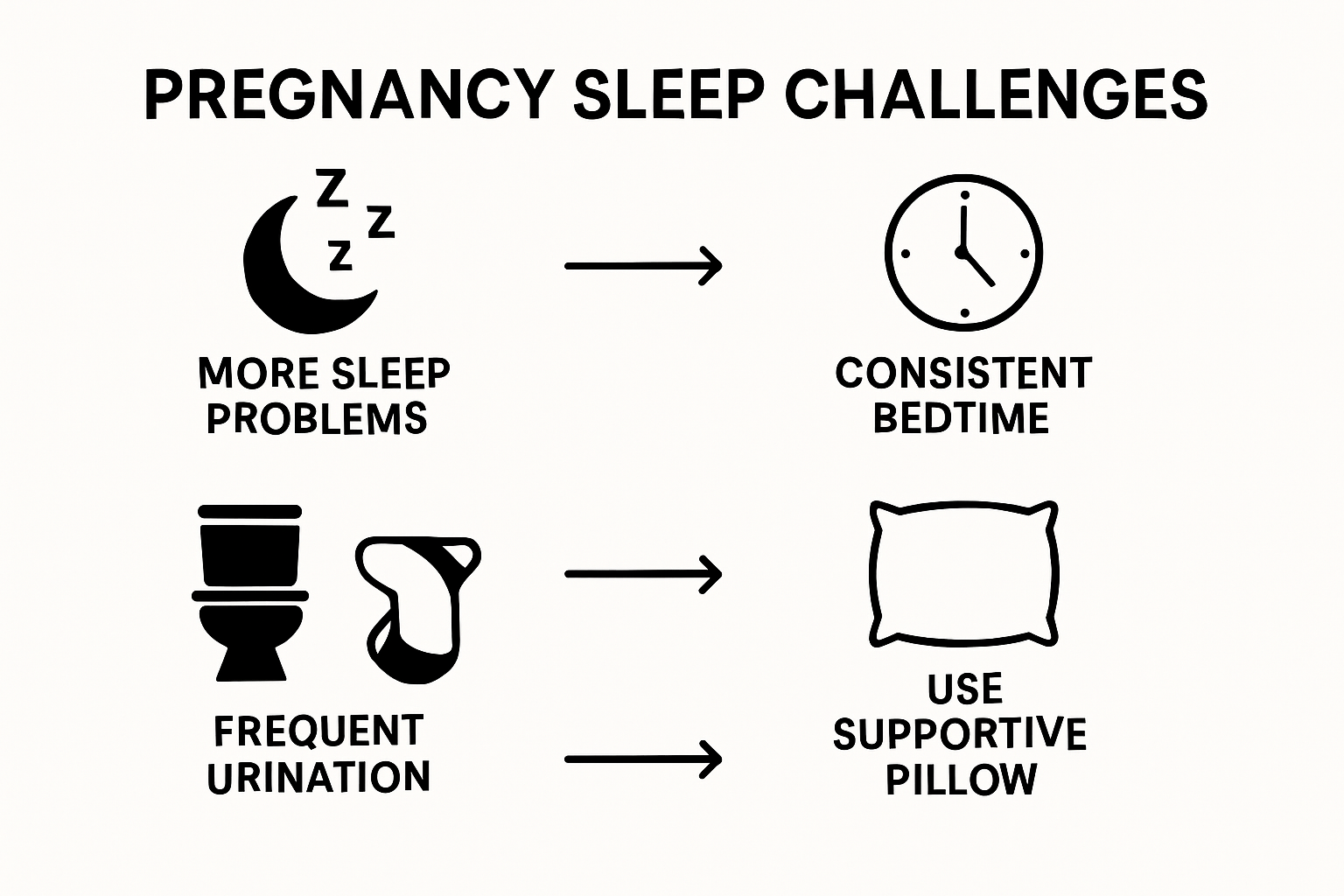
Getting a good night’s sleep sounds simple, but for pregnant women it becomes a daily struggle. Over 75 percent of pregnant women report major sleep problems at some point in their pregnancy. Most people expect cravings or morning sickness, but not the reality that deep, restful sleep might be the toughest thing to find. What surprises many is that sleep issues do more than leave you tired—they actually play a huge part in both mom and baby’s health, making restful nights more important than ever.
Table of Contents
- The Importance Of Sleep During Pregnancy
- Common Sleep Challenges Faced By Pregnant Women
- How Hormones And Physical Changes Affect Sleep
- Practical Sleep Tips For A Better Night’s Rest
- The Role Of Sleep In Maternal And Fetal Health
Quick Summary
| Takeaway | Explanation |
|---|---|
| Sleep is essential for maternal health. | Adequate sleep supports hormone regulation, immune function, and cellular repair during pregnancy. |
| Inadequate sleep risks maternal complications. | Poor sleep may increase the likelihood of gestational diabetes, hypertension, and emotional stress, affecting both mother and baby. |
| Pregnant women face unique sleep challenges. | Hormonal changes and physical discomfort lead to issues like difficulty falling asleep and frequent awakenings, impacting overall rest. |
| Create a conducive sleep environment. | Optimizing room temperature and using supportive pillows can significantly enhance sleep quality and comfort during pregnancy. |
| Practice good sleep hygiene. | Establishing a consistent sleep schedule and minimizing screen time before bed can promote better sleep quality during pregnancy. |
The Importance of Sleep During Pregnancy
Sleep represents a critical component of maternal health during pregnancy, playing a fundamental role in supporting both maternal physiological processes and fetal development. Research from the National Institutes of Health reveals that adequate sleep during pregnancy is far more than just a comfort necessity it is a crucial health requirement with profound implications.
Physiological Impact of Quality Sleep
During pregnancy, sleep becomes a complex biological process that directly influences maternal and fetal well-being. Quality sleep supports critical bodily functions including hormone regulation, immune system maintenance, and cellular repair. Pregnant women experience significant hormonal shifts that can disrupt normal sleep patterns, making consistent rest challenging yet increasingly important.
The physiological demands of pregnancy increase metabolic requirements and cellular stress, which quality sleep helps mitigate. Proper sleep assists in managing inflammation, reducing oxidative stress, and supporting the intricate process of fetal growth. Hormones like progesterone and estrogen undergo substantial fluctuations during pregnancy, and consistent sleep helps stabilize these critical chemical messengers.
Potential Health Consequences of Sleep Disruption
Inadequate sleep during pregnancy is associated with multiple potential health risks. Poor sleep quality can contribute to complications such as:
- Increased risk of gestational diabetes
- Higher likelihood of developing hypertensive disorders
- Potential for prolonged labor duration
- Compromised immune system function
- Elevated emotional stress and potential prenatal depression
Pregnant women who consistently experience disrupted or insufficient sleep may face more significant health challenges. The body requires additional rest to support the complex physiological changes occurring during gestation. Learn more about managing pregnancy stress and supporting your health.
Understanding and prioritizing sleep is not merely about feeling rested it is a fundamental aspect of maternal health that directly impacts both mother and developing child. By recognizing sleep as a critical health intervention, pregnant women can take proactive steps to support their overall well-being during this transformative period.
Common Sleep Challenges Faced by Pregnant Women
Pregnancy transforms a woman’s sleep experience, introducing unique challenges that can significantly impact overall health and well-being. Research indicates that over 75% of pregnant women experience substantial sleep disruptions throughout their pregnancy journey, making understanding these challenges crucial for maternal health.
Hormonal and Physical Disruptions
Hormonal fluctuations during pregnancy create complex physiological changes that directly influence sleep patterns. Progesterone and estrogen levels surge, causing increased fatigue during daytime hours while simultaneously disrupting nighttime sleep quality. These hormonal shifts can lead to significant variations in sleep architecture, including altered sleep stages and reduced deep sleep duration.
Physical transformations compound these challenges. As the body accommodates fetal growth, pregnant women experience multiple physical discomforts that interrupt sleep. Weight gain, expanding abdomen, and shifting center of gravity create difficulties finding comfortable sleeping positions. Increased pressure on the bladder results in frequent nighttime urination, further fragmenting sleep cycles.
Specific Sleep Disturbance Patterns
Sleep challenges during pregnancy manifest through multiple distinct patterns:
- Increased frequency of nocturnal awakenings
- Difficulty falling asleep
- Reduced overall sleep quality
- Heightened daytime sleepiness
- Development of pregnancy-specific sleep disorders
These disruptions are not uniform across pregnancy trimesters. First trimester fatigue often leads to excessive sleepiness, while third trimester physical discomfort tends to cause more significant sleep interruptions. Learn more about managing pregnancy discomforts that can impact sleep quality.
Understanding these sleep challenges enables pregnant women to develop strategies for better rest.
The table below organizes the most common sleep challenges that affect pregnant women and highlights during which trimester(s) they are most likely to occur.
| Sleep Challenge | Description | Most Common Trimester(s) |
|---|---|---|
| Increased nocturnal awakenings | Waking up multiple times during the night | Second, Third |
| Difficulty falling asleep | Trouble initiating sleep due to discomfort or anxiety | All trimesters |
| Reduced overall sleep quality | Lighter, interrupted sleep with less restorative deep sleep | Second, Third |
| Heightened daytime sleepiness | Feeling excessively tired during the day | First |
| Frequent nighttime urination | Needing to urinate often throughout the night | Second, Third |
| Development of pregnancy-specific sleep disorders | Onset of issues like restless leg syndrome | Second, Third |
How Hormones and Physical Changes Affect Sleep
Research from sleep medicine experts reveals the profound impact of hormonal and physiological transformations during pregnancy on sleep patterns. These intricate changes create a complex landscape of sleep disruption that extends far beyond simple fatigue.
Hormonal Mechanisms of Sleep Disruption
Hormones serve as critical regulators of sleep during pregnancy, with progesterone and estrogen playing pivotal roles in dramatically altering sleep architecture. Progesterone levels surge during pregnancy, producing a sedative effect that can cause increased daytime drowsiness while simultaneously fragmenting nighttime sleep. This hormone simultaneously relaxes smooth muscle tissues and influences neurological pathways, creating a dual impact on sleep quality.
Estrogen contributes additional complexity by modulating neurotransmitter systems and influencing circadian rhythms. The fluctuating levels of these hormones can trigger multiple physiological responses that directly interfere with normal sleep cycles, including temperature regulation changes, metabolic shifts, and increased respiratory sensitivity.
Physical Transformations and Sleep Challenges
Physical changes during pregnancy introduce multiple mechanical disruptions to sleep patterns. The expanding uterus and growing fetus create significant bodily challenges that directly impact rest:
- Increased abdominal size altering comfortable sleeping positions
- Heightened pressure on bladder causing frequent nighttime urination
- Shifts in center of gravity creating muscular discomfort
- Potential development of pregnancy-related conditions like restless leg syndrome
- Increased respiratory changes affecting breathing during sleep
These physical transformations become progressively more pronounced as pregnancy advances.
Below is a comparison table summarizing the main hormonal and physical changes during pregnancy and their distinct impacts on sleep quality.
| Change | Description | Impact on Sleep |
|---|---|---|
| Progesterone surge | Increased hormone levels produce a sedative effect | Daytime drowsiness, fragmented sleep |
| Estrogen fluctuations | Alters neurotransmitter systems and circadian rhythms | Changes in sleep cycles, temperature regulation issues |
| Abdominal expansion | Growing uterus and fetus alter body shape | Harder to find comfortable positions |
| Increased bladder pressure | Uterus presses on bladder, especially as pregnancy advances | More frequent nighttime urination |
| Shift in center of gravity | Body balance changes due to fetal growth | Muscle discomfort, harder to rest |
| Respiratory changes | Respiratory system adapts to increased demand | Breathing disruptions during sleep |
Understanding the intricate interplay between hormonal changes and physical transformations provides pregnant women with critical insights into their unique sleep experiences. Recognizing these natural processes can help develop more effective strategies for maintaining rest and overall well-being during this transformative period.
Practical Sleep Tips for a Better Night’s Rest
Research from sleep experts demonstrates that strategic interventions can significantly improve sleep quality during pregnancy. Understanding and implementing specialized techniques can help pregnant women navigate the complex landscape of sleep disruption.
Creating an Optimal Sleep Environment
Designing a sleep-conducive environment is crucial for pregnant women experiencing persistent sleep challenges. Temperature regulation becomes particularly important, as hormonal changes can cause increased body heat and night sweats. Maintaining a cool room temperature between 60-67 degrees Fahrenheit helps promote more consistent sleep patterns.
Ergonomic support plays a critical role in sleep comfort. Investing in specialized pregnancy pillows that support the back, abdomen, and knees can dramatically reduce physical discomfort. These supportive devices help distribute body weight more evenly, alleviating pressure points and reducing nocturnal muscular tension.
Strategic Sleep Hygiene Practices
Sleep hygiene encompasses a range of behavioral and environmental recommendations designed to promote consistent, high-quality rest. Pregnant women can implement several strategic approaches:
- Establish a consistent sleep schedule
- Minimize screen time at least one hour before bedtime
- Create a relaxing pre-sleep ritual
- Use comfortable, breathable sleepwear
- Practice gentle prenatal relaxation techniques
Additionally, moderating fluid intake in the evening can reduce nighttime bathroom disruptions. Consuming smaller quantities of liquid in the hours preceding bedtime helps minimize bladder pressure and subsequent sleep interruptions. Learn more about managing pregnancy discomforts that might impact sleep quality.
By implementing these thoughtful strategies, pregnant women can develop a more comprehensive approach to managing sleep challenges. Recognizing that sleep quality is dynamic and requires personalized adaptation empowers women to take proactive steps toward better rest during this transformative period.

The Role of Sleep in Maternal and Fetal Health
Research examining maternal sleep patterns reveals the profound interconnectedness between maternal sleep quality and comprehensive health outcomes for both mother and developing fetus. Sleep represents more than a restorative process it serves as a critical biological mechanism supporting intricate developmental processes.
Physiological Impact on Maternal Systems
During pregnancy, sleep functions as a fundamental regulatory mechanism influencing multiple physiological systems. Consistent, quality sleep supports critical metabolic processes, hormone regulation, and immune system functionality. Disrupted sleep patterns can trigger cascading physiological responses that potentially impact maternal cardiovascular, endocrine, and immune systems.
Hormonal balance plays a significant role in this complex interaction. Adequate sleep helps maintain appropriate levels of stress hormones like cortisol, which can directly influence fetal development when chronically elevated. The body’s ability to manage inflammation, repair cellular damage, and maintain optimal metabolic function becomes increasingly dependent on consistent, restorative sleep.
Developmental Implications for Fetal Growth
Maternal sleep quality demonstrates direct correlations with multiple fetal developmental markers. Emerging scientific evidence suggests that sleep disruptions can potentially influence:
- Fetal growth rate and birth weight
- Gestational age at delivery
- Potential risk of preterm birth
- Neurological development trajectories
- Immune system maturation
The intricate relationship between maternal sleep and fetal development underscores the importance of comprehensive maternal rest strategies. Learn more about managing pregnancy stress that might impact sleep quality and overall health.
Recognizing sleep as a critical health intervention transforms how pregnant women approach rest. By understanding the multifaceted role of sleep, women can make informed decisions that support not just their personal well-being, but also the complex developmental journey of their unborn child.
Discover Better Sleep and True Leg Comfort During Pregnancy
Struggling with sleepless nights due to discomfort, leg swelling, or restless legs while pregnant is both frustrating and concerning. This article highlights how quality rest is essential for healthy fetal growth, and it uncovers just how much hormonal changes and physical discomfort can disrupt your sleep. If you are feeling worn out by nightly aches or constant pressure in your legs, you are not alone. Managing these symptoms plays a key role in improving your overall rest and supporting your well-being as an expecting mother.
Fit Stockings provides expertly selected compression stockings designed to address pregnancy-related leg discomfort and circulation challenges. Our medical-grade stockings offer gentle, therapeutic support that reduces swelling and eases aching legs, making bedtime and daily routines more comfortable. With a range of styles and sizes from top brands, plus guidance on finding the perfect fit, you can take control of those restless nights starting now. Give yourself the foundation for better sleep and a healthier pregnancy by visiting Fit Stockings today. Experience relief and enjoy free shipping directly to your door.
Frequently Asked Questions
What are some effective sleep tips for pregnant women?
Creating an optimal sleep environment, establishing a consistent sleep schedule, and practicing good sleep hygiene are effective strategies. Consider using supportive pillows and maintaining a cool room temperature to aid rest.
How do hormonal changes during pregnancy affect sleep?
Hormonal fluctuations, particularly in progesterone and estrogen, can disrupt sleep patterns, leading to increased daytime fatigue and nighttime awakenings. These changes can alter sleep architecture, reducing the quality of rest.
What common sleep challenges do pregnant women face?
Pregnant women often encounter challenges such as increased nighttime urination, difficulty finding a comfortable sleeping position, hormonal-induced fatigue, and unique sleep disorders related to pregnancy.
How does sleep quality impact maternal and fetal health?
Adequate sleep supports critical physiological processes in mothers, such as hormone regulation and immune function. It also affects fetal development, influencing growth rates, birth weight, and even neurological outcomes.

